
- Call Now
- +91 9372146545
Services
Gestational Diabetes
Gestational Diabetes
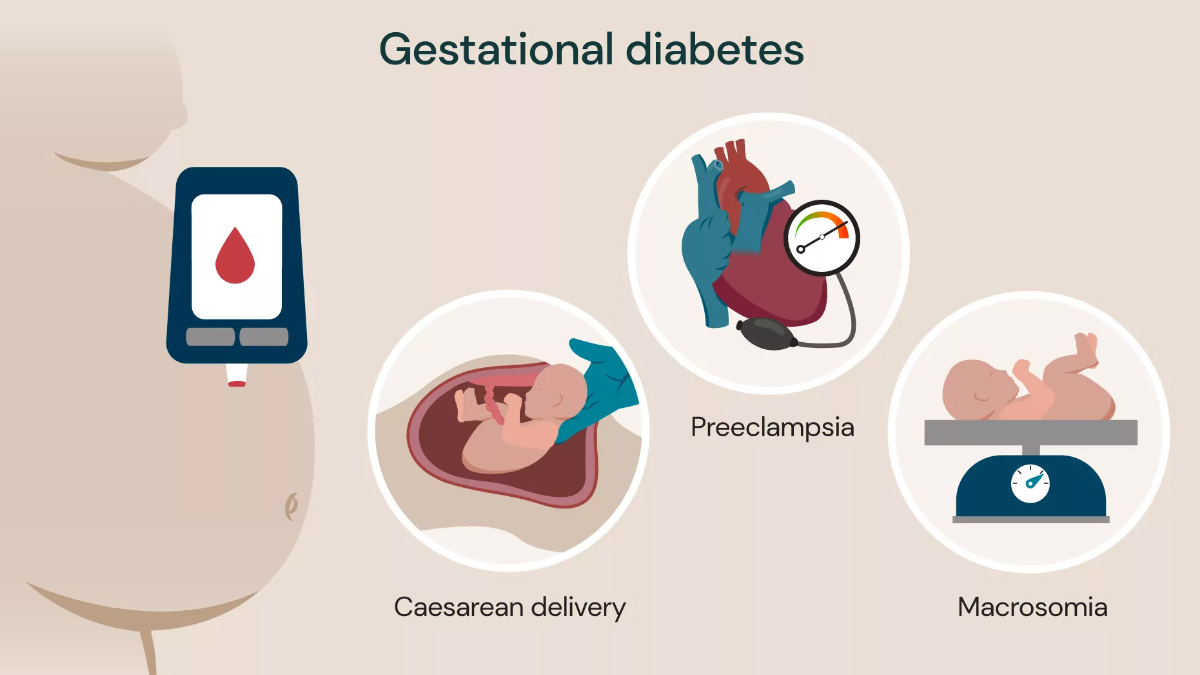
Gestational Diabetes Mellitus (GDM) is a type of diabetes that develops during pregnancy, usually in the second or third trimester, and affects how the body processes glucose. It occurs when hormonal changes in pregnancy impair insulin function, leading to elevated blood sugar levels. Although it often resolves after delivery, gestational diabetes requires careful management to protect both mother and baby.
Women with GDM are at higher risk of complications such as high birth weight (macrosomia), preterm birth, and the need for cesarean delivery. Additionally, both mother and child may have an increased lifetime risk of developing type 2 diabetes. Early detection and management are therefore crucial.
Signs and Symptoms:
Gestational diabetes may not always cause noticeable symptoms, which is why routine screening between 24–28 weeks of pregnancy is recommended. However, some women may experience:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Excessive hunger (polyphagia)
- Fatigue or weakness
- Blurred vision
- Nausea or recurrent infections (such as urinary tract or vaginal infections)
Since these symptoms can sometimes be mistaken for normal pregnancy changes, medical testing is essential for confirmation.
Management:
Management includes lifestyle modifications like balanced nutrition, regular exercise, weight management, and blood glucose monitoring. In some cases, insulin therapy or oral hypoglycemic agents may be necessary. With proper treatment, most women with gestational diabetes can have healthy pregnancies and deliveries.
Regular follow-up and postnatal glucose testing are important, as women with GDM remain at increased risk of developing diabetes in the future.
Services
- Diabetes Management
- Diabetes Counselling
- Diabetes Complications Treatment
- Diabetic Diet & Nutrition Management
- Gestational Diabetes
- Continuous Glucose Monitoring
- Infectious Diseases
- Obesity Management
- Thyroid Disorder
- Metabolic Disorders
- Hypertension
- Heart Diseases
- Neurological Disorders
- Respiratory Diseases
- Gastrointestinal Diseases
